Tuesday, September 19, 2017
The Med-Legal Psych Professor - Cross-Examining Psych Doctors, Tip #101
If you are reading this, chances are that you are an attorney or an insurance professional who has an education, training and experience in those areas. Further, chances are that you do not have education, training or extensive experience as an expert in psychology or psychiatry. As such, you are probably relatively inexperienced about the intricacies of psychological diagnoses and psychological or psychiatric treatment, which puts you at a disadvantage when deciding the best route to take when handling psych reports that are not in your favor. No need to worry any longer. You can access an array of information that will be useful to you in reading psych reports and cross-examining psych doctors who have produced reports not in your favor. Simply subscribe to the Med-Legal Psych Professor blog where you will find over 100 tips with information about psych reports and taking a psych doctor’s testimony.
Tuesday, September 12, 2017
Absence of MCMI-III Scores - Cross-Examining Psych Doctors, Tip #100
The Millon
Clinical Multiaxial Inventory-III (MCMI-III) is the most recent revision of
that test. It contains four scales
capable of providing information about the validity of the test-taker’s
responses. The data from the four validity scales
assess: (1) “Validity” - Did the
individual understand and attend to the content of the questions? (2)
“Debasement” - Did the individual attempt to portray him or herself as having
more troublesome emotional and personal difficulties than exist? (3)
“Desirability” - Did the individual attempt to portray him or herself as being
more morally virtuous, socially attractive and more emotionally well composed
than they are? and, (4) “Disclosure” - Was the individual inclined to be frank
and self-revealing or more likely to be secretive? The MCMI-III is similar to the MMPI-2 in that the test can
only be interpreted to provide information about the individual’s psychological
status if their validity scale scores indicate they completed the test in an
honest and straightforward manner.
However, when the doctor’s report lacks the actual MCMI-III scores the
reader of their report does not know if the test-taker completed the test in an
honest and straightforward manner or attempted to distort their true
presentation. Thus, when you encounter a psych report that is devoid of the
patient’s MCMI-III validity scale scores, you should ask the psych doctor on
cross-examination if there is anything in their report that would allow the
reader of that document to confirm the conclusions they drew from the patient’s
MCMI-III.
The MMPI F(P) Scale - Cross-Examining Psych Doctors, Tip #99
The Minnesota Multiphasic
Personality Inventory (MMPI) is the gold standard of psychological test
batteries used for medical-legal purposes.
The MMPI-2 is the 1989
revision of the original MMPI that dates back more than 70 years and has many
proponents who depend on the test’s validity scales to provide information
about the individual’s test-taking attitudes and credibility. The MMPI-2 is also the most commonly used
version of the MMPI by psychologists and psychiatrists. With regard to the MMPI-2, every
validity and clinical scale performance is described with a T-Score. All T-Scores on the validity scales and the
clinical scales on the MMPI-2 have a mean of 50 and a standard deviation of 10.
In this regard, it should be noted that it is well known and universally
accepted that T-Scores of 65 or larger are clinically significant or
interpretable. In this regard, the F(P) Scale is one of the validity scales of
the MMPI-2. Scores 65 or higher on the F(P) Scale are characteristic of
individuals who are “overreporting
psychopathology” and attempting to portray themselves as having symptoms that
do not exist.
Tuesday, September 5, 2017
The MMPI F(P) Scale - Cross-Examining Psych Doctors, Tip #98
The Minnesota Multiphasic
Personality Inventory (MMPI) is the gold standard of psychological test
batteries used for medical-legal purposes.
The MMPI-2 is the 1989
revision of the original MMPI that dates back more than 70 years and has many
proponents who depend on the test’s validity scales to provide information
about the individual’s test-taking attitudes and credibility. The MMPI-2 is also the most commonly used
version of the MMPI by psychologists and psychiatrists. With regard to the MMPI-2, every
validity and clinical scale performance is described with a T-Score. All T-Scores on the validity scales and the
clinical scales on the MMPI-2 have a mean of 50 and a standard deviation of 10.
In this regard, it should be noted that it is well known and universally
accepted that T-Scores of 65 or larger are clinically significant or
interpretable. In this regard, the F(P) Scale is one of the validity scales of
the MMPI-2. Scores 65 or higher on the F(P) Scale are characteristic of
individuals who are “overreporting
psychopathology” and attempting to portray themselves as having symptoms that
do not exist.
Use of The Oswestry Pain Questionnaire - Cross-Examining Psych Doctors, Tip #98
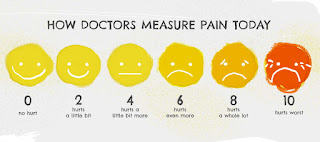
The Oswestry Pain Questionnaire (OPQ) is a
10-item questionnaire that asks an individual to describe their behavior on ten
different variables: Pain Intensity,
Personal Care, Lifting, Walking, Sitting, Standing, Sleeping, Sex Life, Social
Life, and Traveling. In each of the
above noted areas, the test-taker is asked to choose one of the following
categories for themselves: “I can
tolerate the pain I have without having to use pain killers,” “the pain is bad
but I manage without taking pain killers,” “pain killers give complete relief
from pain,” “pain killers give very little relief from pain,” and “pain killers
have no effect on the pain and I do not use them.” Clearly, the OPQ is a self-report questionnaire that has no validity scales for
assessing the individual’s test-taking attitudes or credibility, rendering it
useless in a medical-legal context.
Neuropsychological Medical-Legal Evaluations - Cross-Examining Psych Doctors, Tip #97
Neuropsychology is both an academic
discipline and one of the applied medical arts, often called clinical
neuropsychology. Neuropsychologists are
psychologists who have taken postdoctoral training in the area of
neuropsychology. In the forensic cases
they are typically given referrals by neurologists who depend on their
psychological testing to assess neurological decrements not revealed by the neurologist’s
tools.
While neuropsychological testing can provide the neurologist with
valuable information about a patient’s neurological condition, to use those
testing results to support the conclusion of a “neuropsychological injury” is
to open the door to a double recovery for a single neurological
injury.
Read the Apricot™ and Apply the Advice - Cross-Examining Psych Doctors, Tip #96
I’ve been writing Apricots for about eight
years. Apricots™ are work-product privileged reports designed to help
attorneys cross-examine mental health professionals such as forensic
psychologists, forensic psychiatrists, psychotherapists, social workers
etc. An
Apricot™ describes all of the substantial flaws in a psych report in
jargon-free, non-technical language. An Apricot™ also provides a list of
questions and techniques that will help get those flaws on the record despite
what might be the doctor’s evasive or non-co-operative behavior. In this regard, any attorney who has
commissioned an Apricot™ is strongly urged to read it’s complete contents and
to apply the advice I’ve given in the Apricot™ for the best possible outcomes
with the case. I intentionally put
strong emphasis on reading the contents and apply the advice. For instance, you’ll find in the contents of
my Apricots™ the recommendation that you focus
your questioning on the weakest part of the doctor’s report, which is their
diagnosis. If you don’t take this advice
and pursue a different line of questioning on cross-examination you’ve wasted
the your client’s money that paid for the Apricot™!
Deviating from DSM Terminology - Cross-Examining Psych Doctors, Tip #95
The Diagnostic and Statistical Manual of
Mental Disorders (DSM) provides a variety of mental disorders with a wide
variation of modifiers or specifiers that may be applied to the specific
disorder diagnosed. In addition to
modifiers and specifiers, diagnostic codes are also required in association
with the diagnosis. According to page 1
of the DSM-IV-TR and page 23 of the DSM-5, diagnostic codes are essential for
increased specificity in identifying the intended diagnosis. Unfortunately, some psych doctors choose to
deviate from DSM terminology and create their own diagnosis by adding modifiers
or specifiers that are not outlined or permitted by the DSM. Further, for some unknown reason, some psych
doctors decline to provide a diagnostic code or, even worse, provide diagnostic
codes that do not match their verbal diagnosis which results in a situation where their diagnosis is ambiguous. In
situations where the doctor has created diagnostic uncertainty, during their
deposition you should ask the doctor where
in their report they provided the information about their diagnosis as required
by the DSM.
Subscribe to:
Comments (Atom)